PCOS: 4 Powerful Ways to Improve Symptoms Naturally

Polycystic ovary syndrome (PCOS) sometimes also referred to as PCOD (Polycystic Ovary Disorder) is not just another health buzzword. It’s a complex hormonal condition that affects the ovaries, which produce estrogen, progesterone and small amounts of androgens. In women with PCOS, the balance of these hormones gets disrupted, causing menstrual irregularities, metabolic disruptions, and various other health challenges.
PCOS is far from rare: estimates suggest it affects about 10–15% of women of reproductive age, making it one of the most common endocrine disorders globally.
In this blog, we’ll explore what’s behind this rising trend and, more importantly, how lifestyle-centered changes can make a powerful difference.
Table of Contents
What Drives the Rising Prevalence of PCOS?
Lifestyle, Weight & Insulin Resistance
The rising incidence of PCOS over the past two decades is hardly coincidental. Experts attribute much of it to modern lifestyle factors: chronic stress, sedentary behaviour, poor nutrition, and inadequate sleep. These disrupt the body’s hormonal equilibrium and impair ovarian function. Obesity, now a growing concern worldwide further aggravates the problem. Excess weight often worsens insulin resistance, a core issue in PCOS, and amplifies hormonal imbalances.
Insulin resistance means the body’s cells don’t respond properly to insulin, leading to elevated insulin levels. This can trigger overproduction of androgens (male-type hormones), disturb ovulation, and worsen metabolic health creating a vicious cycle that can be hard to break.
Why PCOS (Not Just PCOD) Matters?
You may often see PCOS and PCOD used interchangeably, but experts treat them differently. Broadly:
PCOD (Polycystic Ovary Disorder) is considered by some as a milder form, one that often responds well to lifestyle improvements like diet and increased activity.
PCOS (Polycystic Ovary Syndrome), by contrast, tends to be more complex, often involving deeper hormonal, metabolic, and even psychological issues which may require more comprehensive management, including medical intervention.
Because PCOS’s roots are multifactorial, involving insulin resistance, hormonal imbalance, genetics, inflammation and lifestyle; a one-size-fits-all approach generally doesn’t work.
Additionally, social stigma around menstrual and reproductive health often makes women reluctant to speak openly about their symptoms delaying diagnosis and care. Normalizing these conversations is a key first step toward better awareness and earlier intervention.
Recognizing the Signs: Common Symptoms to Watch For
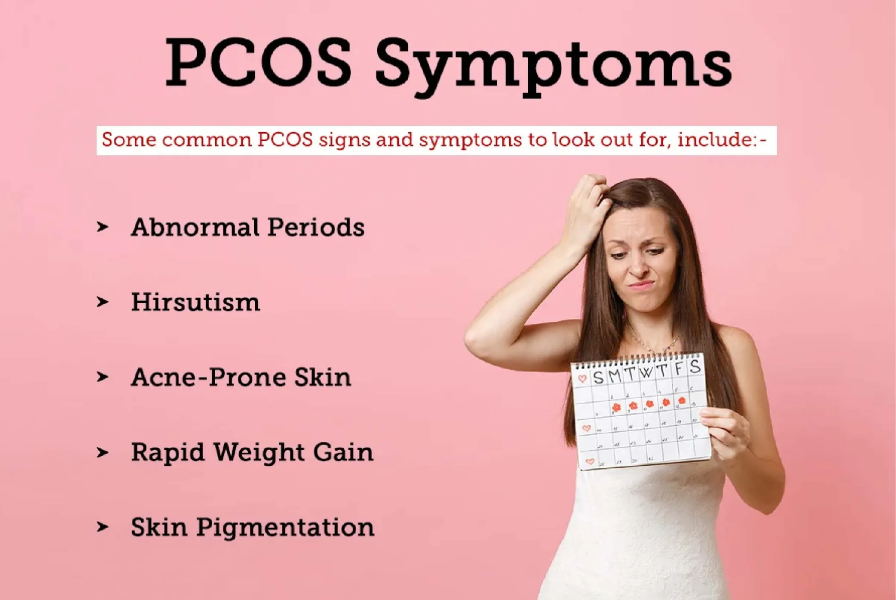
PCOS can manifest in many ways, and symptoms may vary widely from person to person which sometimes makes diagnosis tricky. Some common signs include:
~ Irregular or missed periods; cycles that may be unpredictable, infrequent, or absent.
~ Heavy bleeding when periods do occur.
~ Excess hair growth (hirsutism); e.g., facial hair, hair on chest, abdomen, back.
~ Persistent acne or oily skin, often on face, chest or back.
~ Unexplained weight gain or difficulty losing weight, even with efforts.
~ Thinning hair or hair loss on scalp.
~ Darkened patches of skin (often around neck, underarms, groin).
~ Fatigue, low energy, mood swings or emotional changes.
~ Challenges with fertility or difficulty getting pregnant.
Because symptoms vary and overlap with other conditions, it’s important to consult a doctor if you notice such patterns.
Why Lifestyle Changes Are the First-Line Strategy
While PCOS is complex, research consistently supports lifestyle modification; especially diet, exercise, sleep and stress management as the first line of management.
A comprehensive recent review concluded that combined lifestyle interventions (diet + physical activity + behavioural/psychological support) significantly improve reproductive, metabolic, anthropometric, and psychological outcomes in PCOS.
That said, it’s not “one diet fits all.” The most effective interventions tend to:
- Improve insulin sensitivity.
- Support hormonal balance (e.g. lower androgens, regulate ovulation).
- Help manage weight, body fat, and reduce long-term metabolic risks (like diabetes, cardiovascular disease).
Given the strong influence of lifestyle and the lack of a “magic pill” many experts describe PCOS not as a disease to be “cured,” but as a chronic condition to be managed smartly.
PCOS: 4 Powerful Ways to Improve Symptoms Naturally
While PCOS is complex, lifestyle changes can be transformative in managing its symptoms. Here’s how:
1. Move Your Body: Exercise as Medicine
Regular physical activity isn’t just about weight loss, for PCOS, it’s vital for improving insulin sensitivity, balancing hormones, and supporting reproductive health.
- A recent randomized controlled trial among adolescents with PCOS found that a lifestyle-promotion program (focusing on behaviour change + physical activity + healthy diet) improved anthropometric measures and reduced clinical symptoms.
- According to a 2025 review, combining aerobic and resistance training yields the best results, improving metabolic health and hormonal balance more effectively than either alone.
- Another 2023 case-control study found that women with PCOS who had higher levels of physical activity had significantly lower insulin resistance (measured via HOMA-IR), even when dietary differences were less pronounced.
What to aim for:
- 150 minutes or more of moderate aerobic activity per week + 2–3 sessions of resistance training.
- Include varied activities; brisk walking, cycling, yoga, strength training, etc.
- Make it sustainable: consistency matters more than intensity.
Regular movement not only helps with metabolism, it also improves mood, reduces stress, and supports hormonal regulation.
2. Rethink Your Plate: Nutrition for Hormonal & Metabolic Balance
What you eat has a profound effect on insulin levels, inflammation, hormonal balance — all of which matter deeply in PCOS.
A 2025 systematic review highlighted that diets rich in fiber, omega-3 fatty acids, antioxidants, and low-glycemic-index (GI) foods improved insulin sensitivity and hormonal balance among women with PCOS.
A 2024 network meta-analysis ranking dietary approaches found that the DASH (Dietary Approaches to Stop Hypertension) diet and low-calorie diets were among the most effective in improving BMI and metabolic outcomes for PCOS patients.
Dietary guidelines to consider:
- Emphasize low-GI complex carbohydrates : whole grains (like brown rice, quinoa, oats), millets, legumes; instead of refined carbs and sugars. This helps regulate blood sugar and insulin spikes.
- Include high-fiber foods: vegetables, leafy greens, fruits, whole grains — fiber supports better glucose regulation, reduces insulin resistance, and may even help balance reproductive hormones like LH and FSH.
- Prioritize healthy fats and anti-inflammatory nutrients: omega-3-rich foods (like fatty fish, flaxseeds, chia seeds), nuts, seeds they help lower inflammation, support hormone health and may mitigate androgen effects.
- Opt for balanced meals with lean protein (eggs, fish, legumes), fiber, and healthy fats to support satiety, metabolism, and hormone regulation.
Combined with exercise and other lifestyle changes, a tailored diet can significantly improve outcomes for PCOS.
3. Prioritize Sleep & Stress Management, the Often Overlooked Keys
When it comes to PCOS, it’s not just about what you eat or how you move, your sleep and stress levels matter a lot.
Emerging research supports integrating behavioural and psychological interventions (like stress management, sleep hygiene, mental well-being) along with diet and exercise for a holistic PCOS approach.
A 2024 meta-analysis of mind-body interventions (e.g., yoga, meditation, relaxation) in PCOS found encouraging but mixed results. Some benefits were seen in quality-of-life measures, metabolic parameters, and androgen levels ;though more research is needed.
What to do:
- Aim for 7–8 hours of quality sleep nightly, restful sleep helps regulate hormones, insulin sensitivity, and supports recovery.
- Practice stress-reduction techniques such as yoga, deep breathing, meditation, mindfulness, or even simple leisure activities that help you relax.
- Consider mental-wellness practices as part of your PCOS care routine stress and poor sleep can worsen hormonal imbalance and insulin resistance.
Prioritize Rest, Protect Your Health. Read to know more :
4. Build Long-Term Habits: Holistic & Sustainable Lifestyle Integration
PCOS management isn’t about quick fixes, it’s about sustainable, long-term changes. Recent findings show that lifestyle interventions tailored to individual needs and combined with behavioral support lead to better adherence and outcomes.
Moreover, such comprehensive lifestyle modification doesn’t just improve immediate symptoms it also helps reduce long-term risks like type 2 diabetes, cardiovascular disease, and metabolic syndrome.
How to build sustainable habits:
Set realistic, gradual goals : e.g., small weight loss (5–10%), improved meal quality, 30 mins exercise 4–5× a week, steady sleep schedule. Small wins add up.
Develop a personalized plan that suits your body, preferences, schedule, and challenges. One-size-fits-all rarely works.
Combine diet, exercise, sleep, stress management, and regular check-ins (with yourself or with a supportive community) that synergy leads to better results.
Putting It All Together: A Sample Lifestyle-Centered PCOS Plan
Here’s a weekly roadmap that incorporates the 4 powerful ways, designed for sustainability and real-world life:
| Day | Nutrition | Movement | Sleep & Stress | Notes / Tips |
|---|---|---|---|---|
| Monday | Balanced meals: whole-grains, veggies, lean protein, healthy fats | 30 mins brisk walk + 15 min strength (bodyweight) | Aim for 7-8 hours sleep | Prepare meals ahead to avoid skipping meals |
| Tuesday | Increase fiber (vegetables + legumes) + a serving of omega-3 rich food (e.g. flax seeds, fish) | Yoga / stretching / mobility 30 mins | Sleep: consistent bedtime + no screens 1 hr before bed | Use a food & mood journal to track habits |
| Wednesday | Low-GI carbs, proteins, healthy fats | Aerobic + resistance (light weights) ~40 mins | Relaxation (deep breathing / meditation 10 mins) | Choose enjoyable activities to build consistency |
| Thursday | Antioxidant-rich foods + fiber + healthy fats | Walk or cycling 45 mins | Sleep hygiene + avoid caffeine after 4 pm | Stay hydrated |
| Friday | Balanced diet + protein + fiber | Strength training or HIIT (if comfortable) ~30 mins | Reflect, journal, manage stress | Avoid processed foods / excessive sugar |
| Saturday | Flexible meal but stick to low-GI, whole foods + fibre | Leisure activity: dance, hike or fun sport (~1 hr) | Good sleep + social / mindfulness activity | Social support & community matter for adherence |
| Sunday | Balanced meals + omega-3 + fiber | Light yoga / walk : active recovery | Wind-down routine, early sleep | Plan upcoming week (meals, movement) |
Key principles:
- Focus on consistency over perfection.
- Make gradual changes, sudden extremes are hard to maintain.
- Pay attention to how your body responds and adapt accordingly.
- Combine physical, nutritional and mental-health strategies for the best outcomes.
Check Out Pink Tiger Verified Products and Supplements
Addressing Stigma and Building Awareness
One of the biggest barriers to managing PCOS effectively is social stigma, especially surrounding menstrual health, reproductive health, body image, and “women’s issues.” Many women hesitate to talk about PCOS symptoms, even with close friends or family.
But open dialogue matters, for early diagnosis, emotional support, shared learning, and reducing shame. Here’s how we can change the narrative:
- Encourage honest, stigma-free conversations among women in families, communities, peer groups.
- Use awareness campaigns, workshops, social platforms to share credible information about PCOS.
- Promote body-positive messaging: PCOS affects many women, regardless of body shape or size. It’s not about blame, but about health and empowerment.
- Support access to medical care (gynecologists, endocrinologists), nutritional counselling, mental-health support so women don’t struggle alone.
By fostering understanding and support, we help women feel seen and more empowered to take charge of their health.
Small Steps, Big Changes: The Power of Consistency
PCOS may feel overwhelming sometimes but the good news is: you’re not powerless. Small, consistent lifestyle changes moving a bit more, eating a bit better, sleeping a bit smarter can gradually shift the body’s balance. Over time, these changes accumulate and can lead to meaningful improvements.
Recent research shows exactly that. A 2025 study found lifestyle interventions combining diet, exercise and behaviour change lead to “excellent PCOS symptom control,” especially when tailored to individual needs and supported with behavioural counselling.
So if you’re just starting out don’t be daunted. Begin with one or two changes, build them into habits, and watch over weeks and months as your hormones, energy, mood, and overall health respond.
Final Thoughts & A Gentle Reminder
PCOS is complex and there’s no one-size-fits-all “cure.” But the wealth of recent research suggests that a lifestyle-centered approach remains the most effective, accessible, and long-term way to manage symptoms naturally.
By focusing on:
- regular physical activity,
- balanced, hormone-friendly nutrition,
- quality sleep and stress management,
- sustainable habits and self-care,
you’re not just managing PCOS, you’re investing in your long-term health, hormonal balance, metabolic resilience, and overall well-being.
Frequently Asked Questions (FAQs)
1. What is PCOS and how is it different from PCOD?
PCOS is a hormonal disorder where the ovaries produce higher-than-normal levels of androgens, leading to irregular periods, acne, weight gain, and metabolic issues. PCOD is sometimes considered a milder version where the ovaries develop immature follicles but hormonal imbalance is less severe. Both share symptoms, but PCOS tends to involve stronger metabolic and hormonal impact.
2. What causes PCOS?
PCOS doesn’t have one specific cause, it develops due to a mix of insulin resistance, hormonal imbalances, genetics, inflammation, and certain lifestyle factors. When the body becomes less responsive to insulin, it triggers higher androgen (male hormone) levels, which can disrupt ovulation. A family history of PCOS, unhealthy eating patterns, chronic stress, poor sleep, and weight gain can further increase the risk or worsen symptoms. These factors interact differently for each woman, which is why PCOS looks and feels unique from person to person.
3. What diet is best for PCOS?
A low-GI, high-fiber, anti-inflammatory diet is generally the most effective for women with PCOS because it helps stabilize blood sugar, reduce inflammation, and support hormone balance. This includes focusing on whole grains, legumes, vegetables, fruits with low glycemic load, lean proteins, and healthy fats such as omega-3s from nuts, seeds, and fatty fish. These foods improve insulin sensitivity, which is a key driver of PCOS symptoms, while reducing spikes in glucose that worsen hormonal imbalances. Limiting refined sugars, processed foods, and trans fats can further help regulate cycles, boost energy, and support long-term metabolic health.
4. Why do women with PCOS struggle with weight loss?
Women with PCOS often struggle with weight loss because insulin resistance; one of the most common features of PCOS, makes it harder for the body to use glucose efficiently, causing excess glucose to be stored as fat rather than burned for energy. This contributes to increased hunger, cravings, and a slower metabolic rate. Additionally, hormonal imbalances, especially elevated androgens and cortisol, can affect how the body stores fat and how easily it gains muscle. Chronic low-grade inflammation commonly seen in PCOS further disrupts metabolism, making weight loss more challenging but with the right lifestyle changes, it is absolutely achievable.
5. Is exercise necessary for managing PCOS?
Yes. Regular physical activity; especially a combination of strength training and cardio, improves insulin sensitivity, supports weight management, reduces inflammation, and helps regulate menstrual cycles.
Disclaimer: Please keep your healthcare provider in the loop before introducing any new food item into your lifestyle, especially if you have a medical health condition or are on medications. In case you are allergic to certain foods, please avoid them.
References :
1. Gautam, R., Maan, P., Jyoti, A., Kumar, A., Malhotra, N., & Arora, T. (2025). The Role of Lifestyle Interventions in PCOS Management: A Systematic Review. Nutrients, 17(2), 310. https://doi.org/10.3390/nu17020310
2. Diakosavvas, M., Oyebode, O. & Bhide, P. Weight Management Strategies to Reduce Metabolic Morbidity in Women With Polycystic Ovary Syndrome. Curr Obes Rep 14, 22 (2025). https://doi.org/10.1007/s13679-025-00614-2
3. Mohamed, Amal H. MDa; Albasheer, Osama MDb,*; Ghoniem, Manar Ahmed MSca; Abdalghani, Nagla MDc; Ayish, Fatma MDd; Abdelwahab, Siddig Ibrahim PhDe; Abdelmageed, Maha Murtada MDf; Hakami, Ahlam Mohammed S. MDf; Khormi, Ali Hassan MDf; Altraifi, Ahmed Abdallah MDf; Medani, Isameldin MDf; Chourasia, Uma MDf; Ali, Suhaila A. MDb; Abdelmola, Amani MDb; Ahmed, Anas E. MDb. Impact of lifestyle interventions on reproductive and psychological outcomes in women with polycystic ovary syndrome: A systematic review. Medicine 104(3):p e41178, January 17, 2025. | DOI: 10.1097/MD.0000000000041178
4. Cowan, S., Lim, S., Alycia, C. et al. Lifestyle management in polycystic ovary syndrome – beyond diet and physical activity. BMC Endocr Disord 23, 14 (2023). https://doi.org/10.1186/s12902-022-01208-y
5. Jurczewska, J., Ostrowska, J., Chełchowska, M., Panczyk, M., Rudnicka, E., Kucharski, M., Smolarczyk, R., & Szostak-Węgierek, D. (2023). Physical Activity, Rather Than Diet, Is Linked to Lower Insulin Resistance in PCOS Women—A Case-Control Study. Nutrients, 15(9), 2111. https://doi.org/10.3390/nu15092111
6. Juhász, A.E., Stubnya, M.P., Teutsch, B. et al. Ranking the dietary interventions by their effectiveness in the management of polycystic ovary syndrome: a systematic review and network meta-analysis. Reprod Health 21, 28 (2024). https://doi.org/10.1186/s12978-024-01758-5