Chronic Inflammation: 5 Dangerous Mechanisms Linking Obesity

When we think of inflammation, most of us imagine a swollen ankle, a sore throat, or redness after an injury. That kind of inflammation is obvious and often helpful. But there’s another form of inflammation that doesn’t announce itself with pain or swelling. Instead, it simmers quietly in the background, disrupting metabolism, hormones, and immune balance over time. This is chronic inflammation, and it plays a surprisingly powerful role in obesity and many of today’s lifestyle-related health complications.
In recent years, research has increasingly shown that obesity is not just about excess weight, it is closely tied to a persistent inflammatory state within the body. Understanding this connection helps explain why obesity is often accompanied by insulin resistance, cardiovascular concerns, hormonal imbalances, and even mental fatigue. More importantly, it also shows us how food choices, traditional Indian ingredients, and lifestyle habits can help break this cycle.
Table of Contents
Understanding Chronic Inflammation Beyond the Basics
Inflammation is the body’s natural defense mechanism. It protects us against infections, injuries, and environmental stressors. However, inflammation is not inherently good or bad—it depends on its duration and intensity.
Acute inflammation is short-lived and purposeful. It helps wounds heal, fights infections, and resolves once the threat is gone. Chronic inflammation, on the other hand, lingers for months or even years. It often operates silently, without obvious symptoms, while continuously activating the immune system.
This low-grade inflammatory state interferes with normal cellular communication. Hormones don’t signal effectively, insulin struggles to do its job, and tissues become less responsive to metabolic cues. Over time, this internal imbalance lays the foundation for obesity-related complications.
Multiple studies now confirm that people with excess body fat often show elevated inflammatory markers such as C-reactive protein (CRP), interleukin-6 (IL-6), and tumor necrosis factor-alpha (TNF-α), all hallmarks of chronic inflammation.
The First Dangerous Mechanism: Adipose Tissue as an Inflammatory Organ
One of the most important shifts in obesity research is the understanding that adipose tissue (body fat) is not just a storage depot for excess calories. It is metabolically active and deeply involved in immune signaling.
As fat cells expand to accommodate excess energy intake, they begin to experience stress and oxygen deprivation. This environment triggers the release of inflammatory cytokines, including TNF-α and IL-6. Over time, immune cells, especially macrophages, migrate into fat tissue, further amplifying inflammation.
This creates a feedback loop: larger fat cells promote inflammation, and inflammation promotes further fat accumulation. Research published in Nature Reviews Endocrinology (2025) highlights how inflamed adipose tissue directly interferes with insulin signaling, making weight loss more difficult despite dietary changes.
The Second Mechanism: Reduced Adiponectin and Metabolic Protection Loss
Healthy fat tissue produces adiponectin, a hormone with powerful anti-inflammatory and insulin-sensitizing properties. Adiponectin supports glucose regulation, protects blood vessels, and helps control lipid metabolism.
In obesity, adiponectin levels drop significantly. This loss removes an important protective buffer against chronic inflammation. Lower adiponectin levels are consistently associated with insulin resistance, higher cardiovascular risk, and increased systemic inflammation.
A 2025 cohort study published in The Journal of Clinical Endocrinology & Metabolism found that individuals with lower adiponectin levels had significantly higher CRP and IL-6 concentrations, regardless of calorie intake highlighting inflammation as a core driver rather than just overeating.
The Third Mechanism: Inflammatory Markers That Disrupt Hormones
Chronic inflammation alters the hormonal environment in subtle but impactful ways. Cytokines such as IL-6 and TNF-α interfere with insulin receptors, making cells less responsive to insulin. This promotes higher blood sugar levels and encourages fat storage rather than fat burning.
IL-6 also stimulates the liver to produce C-reactive protein (CRP), a marker widely used to assess systemic inflammation. Elevated CRP is now strongly associated with increased risk of type 2 diabetes and cardiovascular disease.
Emerging 2025 research published in Diabetes Care suggests that reducing inflammatory load independent of weight loss can improve insulin sensitivity. This reinforces the idea that managing chronic inflammation is just as important as calorie control.
The Fourth Mechanism: Gut Inflammation and Metabolic Endotoxemia
Another lesser-known but critical pathway involves the gut. Diets high in refined carbohydrates, sugars, and ultra-processed foods can damage the gut lining, allowing bacterial endotoxins to enter circulation, a process known as metabolic endotoxemia.
These endotoxins activate immune responses and raise inflammatory markers throughout the body. Over time, this contributes to insulin resistance, fat accumulation, and persistent low-grade inflammation.
A 2025 review in Gut Microbes highlighted how diets rich in fiber, polyphenols, and traditional fermented foods help restore gut integrity and reduce inflammatory signaling linked to obesity.
The Fifth Mechanism: Chronic Inflammation and Stress Hormones
Chronic psychological stress further worsens inflammation. Elevated cortisol levels; common in individuals experiencing poor sleep, high stress, and irregular eating patterns, promote abdominal fat storage and inflammatory cytokine production.
Inflammation and stress feed into each other. Inflammatory markers interfere with neurotransmitter balance, increasing fatigue, low mood, and emotional eating tendencies. This cycle makes sustainable weight management increasingly difficult.
Mind–body practices rooted in Indian traditions—such as yoga, pranayama, and meditation, have shown measurable reductions in CRP and IL-6 levels in multiple 2025 clinical studies.
Foods That Quietly Fuel Chronic Inflammation
Modern dietary patterns often unknowingly promote inflammation. Refined carbohydrates like maida-based foods, polished white rice, and sugar-laden sweets cause repeated blood sugar spikes, triggering inflammatory pathways.
Sugary beverages, including packaged fruit juices and sweetened teas, overload the liver with fructose, worsening fat accumulation and inflammation. Processed snacks, instant foods, and preservative-rich pickles introduce additives that disrupt gut health.
Excessive reliance on refined vegetable oils high in omega-6 fatty acids, such as sunflower and soybean oil, can tilt the body toward a pro-inflammatory state when not balanced with omega-3 sources.
Indian Ingredients That Naturally Reduce Inflammation
Traditional Indian diets offer powerful tools to counter chronic inflammation. Leafy greens like spinach, methi, and drumstick leaves are rich in antioxidants that neutralize inflammatory damage.

Turmeric, when paired with black pepper and a healthy fat like ghee, significantly improves curcumin absorption. A 2025 meta-analysis in Phytotherapy Research confirmed curcumin’s role in lowering CRP and TNF-α levels.

Ginger’s bioactive compounds help calm inflammatory pathways, particularly in the gut. Amla, guava, and papaya provide vitamin C, polyphenols, and fiber—essential for immune balance and metabolic health.

Desi ghee, when consumed mindfully, supplies butyrate, a short-chain fatty acid that supports gut lining integrity and reduces inflammation.
Lifestyle Practices That Help Break the Inflammation, Obesity Cycle
Reducing chronic inflammation requires more than food alone. Regular movement, especially walking, yoga, and functional exercises, helps lower inflammatory markers while improving insulin sensitivity.
Sleep plays a non-negotiable role. Poor sleep increases CRP and disrupts hunger hormones. Prioritizing 7–8 hours of consistent sleep supports metabolic repair.
Stress management through pranayama, meditation, grounding, and mindful routines reduces cortisol-driven inflammation. Even simple practices like morning sunlight exposure and eating meals during daylight hours (circadian fasting) can significantly improve inflammatory balance.
The Pink Tiger Approach: Verified Choices for Lower Inflammation
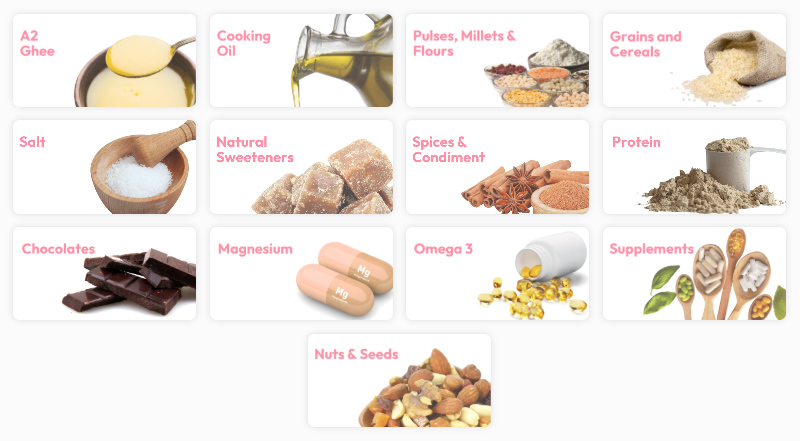
At Pink Tiger, the focus is on helping consumers make informed, safer food and supplement choices, especially in a market flooded with misleading labels. Chronic inflammation often worsens due to hidden additives, pesticide residues, excess heavy metals, and poor-quality fats.
Pink Tiger’s independent testing highlights products verified for label accuracy, contaminant safety, and nutritional integrity. By choosing verified staples; such as clean cooking fats, minimally processed grains, and transparent supplements, individuals can reduce inflammatory triggers that often go unnoticed.
In the long run, reducing chronic inflammation is not about perfection but about consistent, trustworthy choices that support metabolic and immune health.
Check Out ink Tiger Verified Products
Breaking the Inflammation Cycle for Long-Term Health
Chronic inflammation and obesity are deeply interconnected through multiple biological pathways involving adipose tissue behavior, inflammatory markers, gut integrity, hormonal signaling, and stress physiology. Excess fat tissue does more than store energy, it actively releases inflammatory cytokines that disrupt insulin sensitivity and metabolic balance.
At the same time, poor gut health, elevated stress hormones, and sleep disruption further amplify this low-grade inflammation. When weight management focuses only on calorie restriction or the number on the scale, these underlying drivers remain unaddressed, making long-term results difficult to sustain.
A more effective approach looks beyond calories and embraces the wisdom of traditional Indian foods, mindful lifestyle practices, and verified, clean product choices. Nutrient-dense ingredients, balanced fats, gut-supportive foods, regular movement, and stress-reducing rituals work together to calm inflammation at its root. This holistic strategy doesn’t just support healthier weight balance, it protects long-term metabolic efficiency, cardiovascular resilience, and hormonal stability.
Reducing chronic inflammation is not an overnight solution, but it is one of the most impactful steps toward sustainable well-being in today’s fast-paced, high-stress world.
Conclusion
Chronic inflammation sits at the heart of obesity and many modern health challenges, influencing how the body stores fat, regulates hormones, and responds to stress. By shifting focus from quick fixes to inflammation-aware food choices, lifestyle habits, and trusted products, it becomes possible to support lasting metabolic health. Small, consistent changes can gradually calm inflammation, creating a stronger foundation for long-term balance, vitality, and well-being.
Frequently Asked Questions (FAQs)
1. How does chronic inflammation contribute to weight gain even with a controlled diet?
Chronic inflammation disrupts the body’s normal metabolic signaling, making weight gain possible even when calorie intake appears reasonable. Inflammatory cytokines such as IL-6 and TNF-α interfere with insulin receptors, reducing insulin sensitivity. When cells stop responding efficiently to insulin, glucose remains in the bloodstream and is more likely to be stored as fat. Inflammation also alters leptin signaling, the hormone responsible for satiety, leading to impaired hunger cues and overeating without obvious appetite changes. Additionally, chronic inflammation lowers adiponectin levels, a hormone that supports fat breakdown and metabolic flexibility. This creates a biological environment where the body prioritizes fat storage over fat burning. Over time, even balanced diets may not yield expected results unless inflammatory triggers; such as poor sleep, stress, gut imbalance, and ultra-processed foods are addressed alongside nutrition.
2. Why is belly fat more strongly linked to chronic inflammation than other fat stores?
Belly fat, also known as visceral fat, is metabolically more active than subcutaneous fat found under the skin. Visceral fat surrounds vital organs and releases higher levels of inflammatory cytokines like TNF-α and IL-6 directly into the bloodstream. This makes it particularly harmful from an inflammatory perspective. Visceral fat is also more prone to immune cell infiltration, especially macrophages, which amplify inflammatory signaling. Studies show that higher visceral fat levels correlate strongly with elevated CRP levels and insulin resistance. Additionally, visceral fat responds aggressively to stress hormones like cortisol, further increasing inflammation and fat accumulation. This explains why waist circumference is often a stronger predictor of metabolic risk than body weight alone, and why targeting inflammation is crucial for reducing central obesity.
3. Can chronic inflammation affect hormones beyond insulin and weight regulation?
Yes, chronic inflammation affects multiple hormonal pathways beyond insulin. Inflammatory cytokines interfere with thyroid hormone conversion, potentially slowing metabolism and increasing fatigue. They also disrupt cortisol regulation, keeping stress hormones elevated for longer periods, which promotes fat storage and muscle breakdown. In women, chronic inflammation can worsen estrogen imbalance, contributing to conditions like PCOS and irregular cycles. In men, inflammation may reduce testosterone levels, impacting muscle mass and metabolic rate. Additionally, inflammation influences hunger hormones such as leptin and ghrelin, increasing cravings and reducing satiety signals. Over time, this hormonal disruption creates a cycle of low energy, poor metabolic efficiency, and increased fat accumulation. Addressing chronic inflammation can therefore help restore broader hormonal balance, not just support weight management.
4. How does gut health influence chronic inflammation and obesity risk?
The gut plays a central role in regulating inflammation. Diets high in refined carbohydrates, sugars, and additives can weaken the gut lining, allowing bacterial toxins to leak into circulation, a condition known as increased intestinal permeability. These toxins activate immune responses, raising systemic inflammatory markers like CRP. This process, called metabolic endotoxemia, is strongly linked to insulin resistance and fat accumulation. An imbalanced gut microbiome also reduces the production of beneficial short-chain fatty acids like butyrate, which normally help suppress inflammation. Traditional Indian foods rich in fiber, fermented ingredients, polyphenols, and healthy fats support gut integrity and microbial diversity. Improving gut health is one of the most effective ways to reduce chronic inflammation and improve metabolic outcomes.
5. How long does it take to reduce chronic inflammation through lifestyle changes?
Reducing chronic inflammation is a gradual process rather than an overnight fix. Research suggests that measurable reductions in markers like CRP and IL-6 can begin within 4–8 weeks of consistent dietary improvements, better sleep, and regular physical activity. Gut-related inflammation may take longer, often 8–12 weeks, as microbial balance slowly improves. Stress reduction practices such as yoga, pranayama, and meditation can lower cortisol-related inflammation within weeks when practiced consistently. However, long-term benefits depend on sustained habits rather than short-term interventions. Unlike weight loss, inflammation reduction may not always be immediately visible, but improvements in energy, digestion, sleep quality, and metabolic markers often appear earlier. Patience and consistency are key to breaking the inflammation–obesity cycle.
Disclaimer : This content is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider for any questions or concerns regarding your health.
Reference :
1. Zalagkitis, C., Philippou, A., Karatzanos, E., Metsios, G., & Dinas, P. C. (2025). Combined effects of physical activity and diet on chronic inflammation of overweight/obese children and adolescents: A systematic review and meta-analysis. Journal of sports sciences, 43(22), 2841–2857. https://doi.org/10.1080/02640414.2025.2561349
2. Bulmer, C., & Avenell, A. (2025). The effect of dietary weight-loss interventions on the inflammatory markers interleukin-6 and TNF-alpha in adults with obesity: A systematic review and meta-analysis of randomized controlled clinical trials. Obesity reviews : an official journal of the International Association for the Study of Obesity, 26(7), e13910. https://doi.org/10.1111/obr.13910
3. Neira, G., Gómez-Ambrosi, J., Cienfuegos, J.A. et al. Increased expression of IL-1β in adipose tissue in obesity influences the development of colon cancer by promoting inflammation. J Physiol Biochem 81, 471–482 (2025). https://doi.org/10.1007/s13105-024-01048-5
4. Wang, C., Yi, Z., Jiao, Y., Shen, Z., Yang, F., & Zhu, S. (2023). Gut Microbiota and Adipose Tissue Microenvironment Interactions in Obesity. Metabolites, 13(7), 821. https://doi.org/10.3390/metabo13070821
5. Newman, N.K., Zhang, Y., Padiadpu, J. et al. Reducing gut microbiome-driven adipose tissue inflammation alleviates metabolic syndrome. Microbiome 11, 208 (2023). https://doi.org/10.1186/s40168-023-01637-4
6. Lee, Y. M., & Kim, Y. (2024). Is Curcumin Intake Really Effective for Chronic Inflammatory Metabolic Disease? A Review of Meta-Analyses of Randomized Controlled Trials. Nutrients, 16(11), 1728. https://doi.org/10.3390/nu16111728
7. Naghsh, N., Musazadeh, V., Nikpayam, O., Kavyani, Z., Moridpour, A. H., Golandam, F., Faghfouri, A. H., & Ostadrahimi, A. (2023). Profiling Inflammatory Biomarkers following Curcumin Supplementation: An Umbrella Meta-Analysis of Randomized Clinical Trials. Evidence-based complementary and alternative medicine : eCAM, 2023, 4875636. https://doi.org/10.1155/2023/4875636
8. Feng J (2025) Role of curcumin in altering gut microbiota for anti-obesity and anti-hyperlipidemic effects. Front. Microbiol. 16:1625098. doi: 10.3389/fmicb.2025.1625098