Type 2 Diabetes: 5 Essential Steps to Reclaim Your Health

Diabetes is often described as a silent epidemic, a condition that progresses quietly until complications begin to surface. Over the past decade, diabetes has transformed from a medical concern into a public health emergency. India now ranks second globally with more than 74 million people living with Diabetes, highlighting the urgent need for awareness, prevention, and practical strategies for reversal.
The encouraging truth? Type 2 Diabetes is largely preventable and, in many cases, reversible. With targeted lifestyle interventions and consistent habits, millions can improve metabolic health and reclaim control over their bodies.
This comprehensive guide breaks down the science, the lifestyle shifts, and the five essential steps you can begin today.
Table of Contents
India’s Diabetes Burden: Beyond Statistics

India’s relationship with Diabetes is complex. According to recent projections, one in every six diabetics globally is Indian. While genes do play a role, they cannot fully explain this staggering rise. The real culprits lie in our modern-day choices:
- Ultra-processed foods and excessive carbohydrate intake
- Sedentary routines dominated by screens
- Chronic stress from fast-paced lifestyles
- Poor sleep hygiene
- Declining levels of physical activity compared to previous generations
The silver lining is that all these factors are modifiable. Diabetes is not simply a diagnosis; it’s a wake-up call, a sign that the body’s metabolic systems need support. With the right lifestyle changes, the trajectory of Type 2 Diabetes can shift dramatically.
Type 2 Diabetes: A Lifestyle-Centric Disorder
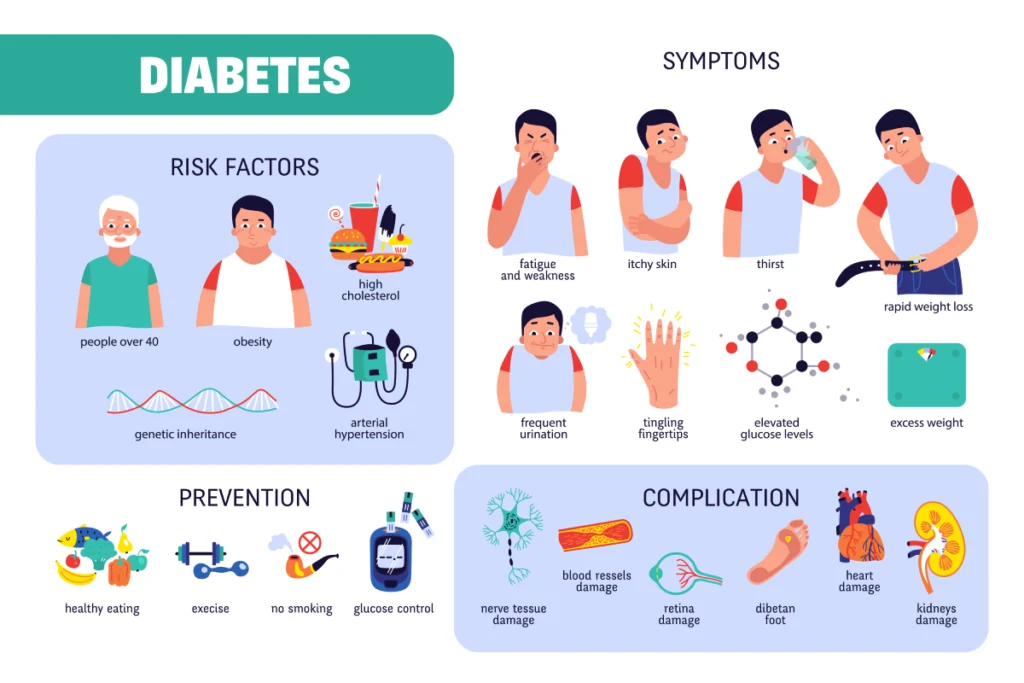
Type 2 Diabetes is fundamentally a metabolic condition driven by insulin resistance, where cells stop responding effectively to insulin. This causes elevated blood glucose levels and sets the stage for complications such as heart disease, kidney damage, nerve issues, and vision problems.
Unlike autoimmune conditions or genetic disorders, Type 2 Diabetes is deeply influenced by daily lifestyle choices. That’s what makes it both challenging and empowering. The same habits that contribute to Diabetes can be reshaped to support healing.
Recent studies from 2024–2025 reinforce that early lifestyle interventions produce significant improvements in:
- Insulin sensitivity
- Fasting glucose
- Weight management
- Inflammation levels
- Liver health
- Gut microbiome diversity
Small, consistent changes can shift metabolic patterns and even reverse Diabetes in many individuals.
The 5 Essential Steps to Reclaim Your Health
Below are the five foundational steps backed by modern clinical research that can help you manage, improve, and potentially reverse Type 2 Diabetes.
Step 1: Mindful Eating – Nourish Instead of Restrict
Nutrition is the most powerful tool for diabetes reversal. Mindful eating is not a diet; it’s an approach that focuses on quality, balance, and awareness.
Choose Whole, Unprocessed Foods
Foods close to nature improve blood sugar control:
- Fresh vegetables
- Whole grains like brown rice, millets, oats
- Lentils and legumes
- Lean proteins (eggs, chicken, fish, paneer, tofu)
- Healthy fats (nuts, seeds, olive oil, ghee in moderation)
These foods support:
- Better gut health
- Reduced inflammation
- Improved insulin sensitivity
- Longer-lasting energy
Avoid Hidden Sugars and Ultra-Processed Foods
Packaged foods often contain:
- Added sugars
- Artificial sweeteners
- High-fructose corn syrup
- Refined flours
- Trans fats
Reading labels helps you avoid ingredients that spike blood sugar or burden the pancreas.
Practice Portion and Timing Awareness
- Avoid late-night eating
- Ensure balanced plates (protein + fiber + healthy fats + slow carbs)
- Maintain consistent meal timings to stabilize glucose levels
2024 nutritional research shows that consistent eating windows and balanced macro distribution significantly improve glycemic control.
Step 2: Move Daily – Unlock Your Body’s Natural Insulin Sensitivity
Movement is medicine, perhaps the most underrated one.
Regular physical activity directly improves how cells use glucose. Even a 10–15 minute walk after meals can lower post-meal spikes by up to 30%, according to new clinical studies.
Recommended Movement Practices
- Daily walking: Aim for 7,000–10,000 steps
- Strength training: 2–3 times per week
- Cardio: Brisk walking, cycling, swimming
- NEAT movement: Standing more, stretching, simple at-home movements
Strength training is particularly beneficial because muscles act like glucose storage units. The more muscle you build, the more insulin responsive your body becomes.
Consistency Beats Intensity
You don’t need intense workouts. What matters most is:
- Small movements
- Repeated daily
- Integrated into life
Movement reduces cravings, improves sleep, enhances mood, and strengthens metabolism.
Step 3: Prioritize Stress and Sleep Management
Chronic stress is an invisible driver of Diabetes. When stressed, the body releases cortisol, which increases blood sugar levels as a survival mechanism.
High stress can mimic the effects of poor diet, making blood sugar harder to control even if eating well.
Addressing Stress: Simple, Effective Practices
- 5 minutes of deep breathing
- Meditation or mindfulness apps
- Journaling
- Gentle yoga
- Spending time in nature
- Digital detox periods
These practices reduce cortisol, improve insulin sensitivity, and balance the nervous system.
The Sleep-Diabetes Connection
Poor sleep disrupts:
- Appetite hormones (ghrelin and leptin)
- Insulin response
- Metabolism
- Cravings
- Inflammation
Aim for 7–8 hours of quality sleep, maintain a nighttime routine, avoid screens late at night, and keep your bedroom cool and dark.
Step 4: Hydrate Smartly – Support Metabolism Naturally
Hydration is often overlooked, yet it significantly impacts metabolic health.
Why Hydration Matters
- Helps kidneys flush excess glucose
- Improves digestion
- Reduces cravings
- Supports cellular repair
- Enhances metabolism
Smart Hydration Choices
- Water
- Herbal teas (ginger, cinnamon, green tea)
- Infused water (lemon, mint, cucumber)
Avoid sugary drinks:
- Sodas
- Packaged juices
- Sweetened coffees
- Milkshakes
- Energy drinks
These cause immediate spikes in blood sugar and contribute to insulin resistance.
Step 5: Embrace Holistic Healing – Fix the Root, Not Just the Symptoms
Managing Diabetes goes beyond controlling blood sugar with medications. A holistic approach looks deeper at inflammation, hormones, gut health, nutrient deficiencies, and emotional wellbeing.
Key Areas of Holistic Healing
- Gut health: A diverse microbiome improves glucose control
- Anti-inflammatory foods: Turmeric, ginger, omega-3-rich foods
- Nutrient support: Magnesium, chromium, vitamin D, B12 (assess deficiencies)
- Balanced hormones: Especially cortisol, thyroid hormones, and insulin
Instead of chasing symptoms, holistic healing helps reprogram the body’s metabolic engine.
The Power of Small, Consistent Actions
One of the biggest misconceptions is thinking you need to overhaul your life to reverse Diabetes. In reality, sustainable progress comes from small actions done consistently, such as:
1. Choosing a home-cooked meal over a processed one
Switching to home-cooked meals is one of the most impactful steps you can take for better blood sugar control. Processed foods often contain hidden sugars, refined flours, unhealthy fats, preservatives, and additives that spike glucose and increase inflammation. When you cook at home, you control the ingredients, the portion sizes, and the cooking methods. Simple meals like dal, sabzi, eggs, stir-fried vegetables, or fresh salads nourish the body with fiber, protein, and micronutrients that keep blood sugar stable. Even replacing just one processed meal a day with a wholesome home-cooked option can improve metabolic health over time.
2. Adding a 10-minute walk post dinner
A short walk after dinner acts like a natural glucose-lowering tool. After eating, blood sugar naturally rises, and a gentle walk helps your muscles use that circulating sugar for energy. Studies show that just 10–15 minutes of walking after meals can reduce post-meal glucose spikes by up to 30%, improving insulin sensitivity and sleep quality. It doesn’t need to be an intense workout, just a relaxed stroll in your home, building, or nearby park. This small habit, practiced consistently, can significantly improve overnight blood sugar levels.
3. Practicing 5 minutes of breathing
Five minutes of intentional, deep breathing can reset your nervous system and lower stress hormones that interfere with blood sugar control. When you take slow, mindful breaths, your body shifts from “fight or flight” to “rest and digest,” reducing cortisol and helping insulin work more effectively. Breathing exercises like box breathing, diaphragmatic breathing, or simple slow inhales and exhales calm the mind, improve focus, and reduce cravings triggered by stress. It’s a small commitment but a powerful tool for emotional and metabolic balance.
4. Drinking 2–3 extra glasses of water
Hydration plays a bigger role in diabetes management than most people realize. Drinking more water helps the kidneys flush out excess glucose through urine, supports digestion, improves metabolism, and reduces false hunger signals. Often, sugar cravings or afternoon fatigue are actually signs of dehydration. By consciously adding 2–3 extra glasses of water to your daily routine; especially between meals, you help your body maintain optimal blood viscosity and glucose balance. Herbal teas or infused water can also be refreshing, low-calorie alternatives.
5. Sleeping 30 minutes earlier
Going to bed just 30 minutes earlier may seem small, but it can dramatically improve metabolic health. Lack of sleep raises cortisol, disrupts hunger hormones, increases cravings, and makes the body more insulin resistant the next day. By extending your sleep window even slightly, you give your body more time to repair, balance hormones, and stabilize blood sugar. Over weeks and months, this small shift leads to better energy, reduced morning glucose levels, improved mood, and fewer unhealthy food choices driven by fatigue.
These micro-habits stack up and create powerful metabolic shifts.
Research shows that even a 5-7% reduction in body weight can significantly improve insulin sensitivity and lower blood sugar levels.
Pink Tiger Verified Products: Choose Safer, Cleaner Nutrition
When managing or reversing Type 2 Diabetes, the quality of your food and supplements matters. Pink Tiger–verified products offer an added layer of trust because they undergo independent lab testing for contaminants, hidden sugars, pesticides, heavy metals, and misleading labels.
Choosing Pink Tiger approved options helps ensure you’re consuming clean, honest, and safe products that support better blood sugar control and overall metabolic health.
Final Thoughts: You Can Reclaim Your Health
Type 2 Diabetes is not a life sentence. It’s a signal that your body needs care, nourishment, and balance. With consistency, mindful choices, and the right lifestyle habits, you can dramatically improve your health.
Start with one step; just one.
Then add another.
And another.
Small steps today lead to remarkable transformations tomorrow.
Your journey to health begins exactly where you are.
Frequently Asked Questions (FAQs)
1. Can Type 2 Diabetes really be reversed?
Yes, Type 2 Diabetes can often be reversed or significantly improved, especially when addressed early. Reversal means bringing blood sugar levels back into a healthy range without relying heavily on medication. This is usually achieved through sustained lifestyle changes such as improved nutrition, regular physical activity, weight loss, stress reduction, and better sleep habits. While not everyone experiences full reversal, particularly those with long-standing diabetes, many people see dramatic improvements by consistently following evidence-based practices.
2. How long does it take to see improvements in blood sugar levels?
Improvements can begin within as little as 2-4 weeks when you consistently make positive lifestyle changes. Many individuals notice better fasting glucose, fewer post-meal spikes, increased energy, reduced cravings, and improved digestion. However, deeper metabolic improvements, such as enhanced insulin sensitivity and reduced inflammation, generally take 3-6 months. The timeline varies depending on factors like age, weight, activity levels, stress, sleep quality, and how closely the recommended habits are followed.
3. Do I need to follow a strict diet to manage Diabetes?
No, you don’t need a strict or restrictive diet to manage Type 2 Diabetes. What matters far more is eating real, whole foods in balanced portions. The goal is to focus on vegetables, proteins, good fats, and slow-digesting carbs while avoiding refined sugars, processed foods, and junk snacks. Extreme diets may offer quick results but are rarely sustainable. Instead, a flexible, mindful, and balanced approach helps stabilize blood sugar while still allowing you to enjoy food without feeling deprived.
4. Can walking alone help lower blood sugar?
Yes, walking is one of the simplest and most effective tools for managing Diabetes. Research shows that even a 10–15 minute walk after meals can significantly lower post-meal glucose levels by helping muscles absorb circulating sugar. Walking improves insulin sensitivity, boosts circulation, reduces stress, and supports weight management. While adding strength training and other exercises can provide even greater benefits, daily walking alone can make a meaningful difference in controlling Diabetes.
5. Why is stress management important for Diabetics?
Stress triggers the release of cortisol and adrenaline, hormones that raise blood sugar as part of the body’s natural “fight-or-flight” response. When stress becomes chronic, these hormones remain elevated, making it harder for insulin to work effectively. This can lead to persistent high blood sugar levels even when diet and exercise are on track. Incorporating simple stress-relief practices like deep breathing, meditation, gentle yoga, journaling, or spending time in nature can significantly support more stable glucose levels and overall emotional wellbeing.
Disclaimer: Please keep your healthcare provider in the loop before introducing any new food item or beauty product into your lifestyle, especially if you have a medical health condition or are on medications. In case you are allergic to certain foods, please avoid them.
References:
1. Lim, E.L., Hollingsworth, K.G., Aribisala, B.S. et al. Reversal of type 2 diabetes: normalisation of beta cell function in association with decreased pancreas and liver triacylglycerol. Diabetologia 54, 2506–2514 (2011). https://doi.org/10.1007/s00125-011-2204-7
2. Sagastume, D., Siero, I., Mertens, E., Cottam, J., Colizzi, C., & Peñalvo, J. L. (2022). The effectiveness of lifestyle interventions on type 2 diabetes and gestational diabetes incidence and cardiometabolic outcomes: A systematic review and meta-analysis of evidence from low- and middle-income countries. EClinicalMedicine, 53, 101650. https://doi.org/10.1016/j.eclinm.2022.101650
3. Zhang, Y., Yang, Y., Huang, Q., Zhang, Q., Li, M., & Wu, Y. (2023). The effectiveness of lifestyle interventions for diabetes remission on patients with type 2 diabetes mellitus: A systematic review and meta-analysis. Worldviews on evidence-based nursing, 20(1), 64–78. https://doi.org/10.1111/wvn.12608
4. Magkos, F., Hjorth, M.F. & Astrup, A. Diet and exercise in the prevention and treatment of type 2 diabetes mellitus. Nat Rev Endocrinol 16, 545–555 (2020).https://doi.org/10.1038/s41574-020-0381-5
5. Hallberg, S. J., Gershuni, V. M., Hazbun, T. L., & Athinarayanan, S. J. (2019). Reversing Type 2 Diabetes: A Narrative Review of the Evidence. Nutrients, 11(4), 766. https://doi.org/10.3390/nu11040766
6. The essential role of exercise in the management of type 2 diabetes John P. Kirwan, Jessica Sacks, Stephan Nieuwoudt Cleveland Clinic Journal of Medicine Jul 2017, 84 (7 suppl 1) S15-S21; DOI: 10.3949/ccjm.84.s1.03
7. Thomas D, Elliott EJ, Naughton GA. Exercise for type 2 diabetes mellitus. Cochrane Database of Systematic Reviews 2006, Issue 3. Art. No.: CD002968. DOI:10.1002/14651858.CD002968.pub2.
8. Dong, C., Liu, R., Huang, Z. et al. Effect of exercise interventions based on family management or self-management on glycaemic control in patients with type 2 diabetes mellitus: a systematic review and meta-analysis. Diabetol Metab Syndr 15, 232 (2023).https://doi.org/10.1186/s13098-023-01209-4
9. Goyal Mehra, C., Raymond, A.M. & Prabhu, R. A personalized multi-interventional approach focusing on customized nutrition, progressive fitness, and lifestyle modification resulted in the reduction of HbA1c, fasting blood sugar and weight in type 2 diabetes: a retrospective study. BMC Endocr Disord 22, 290 (2022). https://doi.org/10.1186/s12902-022-01212-2
10. Knowler, W. C., Barrett-Connor, E., Fowler, S. E., Hamman, R. F., Lachin, J. M., Walker, E. A., Nathan, D. M., & Diabetes Prevention Program Research Group (2002). Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. The New England journal of medicine, 346(6), 393–403.https://doi.org/10.1056/NEJMoa012512
11.